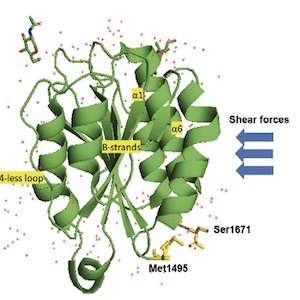
The von Willebrand factor-ADAMTS-13 axis: a two-faced Janus in bleeding and thrombosis
Published: April 26 2022
Abstract Views: 1969
PDF: 341
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- Juan Eirís, Marina Suárez-Terrón, Pablo Granados, David Martínez-Campuzano, Ana Rosa Cid, Saturnino Haya, Santiago Bonanad, Allopurinol-induced acquired von Willebrand syndrome , Bleeding, Thrombosis and Vascular Biology: Vol. 2 No. 4 (2023)
- Boris Shenkman, Ivan Budnik, Yulia Einav, Interaction between adenosine diphosphate receptors and protein-kinase C isoforms in platelet adhesion under flow condition , Bleeding, Thrombosis and Vascular Biology: Vol. 2 No. 1 (2023)
- Luca D'Ambrosio, Maurizio Forte, Giacomo Frati, Sebastiano Sciarretta, Role of platelet autophagy in cardiovascular diseases , Bleeding, Thrombosis and Vascular Biology: Vol. 3 No. 2 (2024)
- Stefania Momi, Giuseppe Guglielmini, Giulia Ciarroca Taranta, Elisa Giglio, Angela Monopoli, Paolo Gresele, A nitric oxide-donor pravastatin hybrid drug exerts antiplatelet and antiatherogenic activity in mice , Bleeding, Thrombosis and Vascular Biology: Vol. 1 No. 2 (2022)
- Giovanni L. Tiscia, Donatella Colaizzo, Antonio De Laurenzo, Filomena Cappucci, Lucia Fischetti, Elena Chinni, Mario Mastroianno, Giovanni Favuzzi, Massimo Carella, Elvira Grandone, Thrombin generation assay in COVID-19 patients shows a hypocoagulable pattern , Bleeding, Thrombosis and Vascular Biology: Vol. 3 No. 3 (2024)
- Pantep Angchaisuksiri, Wolfram Ruf, Jeffrey Weitz, Sam Schulman, Guy A. Young, A commitment to global collaboration, welcoming international participation and advancing science for the benefit of patients , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. 2 (2025)
- Francesca Santilli, Paola Simeone, Rossella Liani, Inflammation, platelets and diabetes , Bleeding, Thrombosis and Vascular Biology: Vol. 2 No. 2 (2023)
- Daniela Poli, Riccardo Tartaglia, Doris Barcellona , Paolo Bucciarelli , Antonio Ciampa, Elvira Grandone, Giuseppe Malcangi, Giuseppe Rescigno, Vincenzo Toschi, Sophie Testa, Alessandro Squizzato, Attitude to clinical research among health professionals affiliated with the Italian Federation of Centers for the Diagnosis of Thrombotic Disorders and the Surveillance of the Antithrombotic Therapies (FCSA) , Bleeding, Thrombosis and Vascular Biology: Vol. 2 No. 1 (2023)
- Domenico Prisco, Irene Mattioli, Raffaele De Caterina, Alessandra Bettiol, The new era of anticoagulation: factor XI and XII inhibitors , Bleeding, Thrombosis and Vascular Biology: Vol. 2 No. 2 (2023)
- Marcello Di Nisio, Matteo Candeloro, Nicola Potere, Ettore Porreca, Jeffrey I. Weitz, Factor XI inhibitors: a new option for the prevention and treatment of cancer-associated thrombosis , Bleeding, Thrombosis and Vascular Biology: Vol. 3 No. s1 (2024): 12th ICTHIC
1-10 of 50
Next
You may also start an advanced similarity search for this article.