An ecological alliance against air pollution and cardiovascular disease

All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
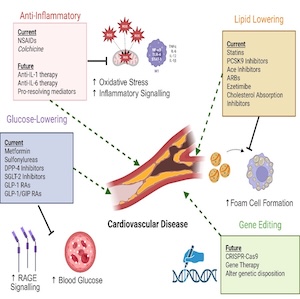
This narrative review article summarizes the strong available evidence that casually links indoor and outdoor air pollution to cardiovascular disease. It also discusses as a possible approach to mitigate this ubiquitous risk factor the use in the household of ornamental potted plants, and their variable degree of effectiveness for the removal of different indoor pollutants such as volatile organic compounds (formaldehyde, benzene, toluene, xylene). Thus, the choice of the plants should be tailored to the types and concentrations of the pollutants present in each household. Outdoor air is less polluted than indoor air in terms of concentrations of the gaseous (NO2) and particulate components (PM10, PM2.5, PM0.1), but it does hamper to a higher extent health because a large fraction of the population is inevitably exposed at the time of breezing. Being cognizant of the difficulties currently encountered in the attempts to mitigate the major sources of ambient air pollution (vehicle traffic and domestic heating) a strategy based upon a massive increase of green spaces in urban areas has been shown not only to positively mitigate air pollution but also improve life expectancy, general health and resilience.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.
Most read articles by the same author(s)
- Pier Mannuccio Mannucci, Gene transfer in hemophilia A: not cogent yet , Bleeding, Thrombosis and Vascular Biology: Vol. 1 No. 1 (2022)
- Pier Mannuccio Mannucci, Growing weapons to fight hemophilia , Bleeding, Thrombosis and Vascular Biology: Vol. 2 No. 1 (2023)