Crosstalk between hemostasis inhibitors and cholesterol biomarkers in multiple sclerosis
Submitted: 31 May 2022
Accepted: 8 September 2022
Published: 17 October 2022
Accepted: 8 September 2022
Abstract Views: 2221
PDF: 228
Supplementary Files: 54
Supplementary Files: 54
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Most read articles by the same author(s)
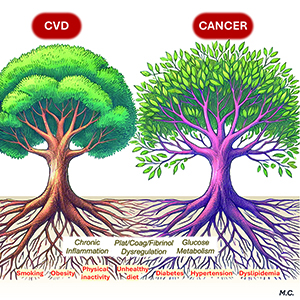
- Marcello Baroni, Paolo Ferraresi, Nicole Ziliotto, Daria Bortolotti, Pierfilippo Acciarri, Nicola Martinelli, Giovanna Marchetti, Matteo Coen, Francesco Bernardi, Protein S on the surface of plasma lipoproteins: a potential mechanism for protein S delivery to the atherosclerotic plaques? , Bleeding, Thrombosis and Vascular Biology: Vol. 1 No. 3 (2022)
- Loredana Bury, Alessio Branchini, Francesco Bernardi, Paolo Gresele, Platelet transcriptomic changes in myocardial infarction are sex and clinical subtype-related: a step forward towards precision medicine? , Bleeding, Thrombosis and Vascular Biology: Vol. 4 No. 1 (2025)
Similar Articles
- Federica Mancazzo, Antonia Vitulli, Lavinia Dirienzo, Concetta T. Ammollo, Fabrizio Semeraro, Mario Colucci, Influence of emicizumab on protein C-mediated clotting regulation , Bleeding, Thrombosis and Vascular Biology: Vol. 2 No. 4 (2023)
- Anna Maria Gori, Eleonora Camilleri, Alessia Bertelli, Angela Rogolino, Francesca Cesari, Elena Lotti, Tommaso Capobianco, Walther Iannotti, Betti Giusti , Rossella Marcucci, Pleiotropic effects of anti-thrombotic therapies: have direct oral anticoagulants any anti-inflammatory effect? , Bleeding, Thrombosis and Vascular Biology: Vol. 1 No. 3 (2022)
- Roberta Parisi, Simona Costanzo, Romy de Laat-Kremers, Augusto Di Castelnuovo, Amalia De Curtis, Teresa Panzera, Mariarosaria Persichillo, Chiara Cerletti, Giovanni de Gaetano, Maria Benedetta Donati, Licia Iacoviello, Bas de Laat , for the Moli-sani Study Investigators, Plasma fibrinogen levels and all-cause and cause-specific mortality in an Italian adult population: results from the Moli-sani study , Bleeding, Thrombosis and Vascular Biology: Vol. 2 No. 1 (2023)
- Kamran Abbasi, Parveen Ali, Virginia Barbour, Kirsten Bibbins-Domingo, Marcel G.M. Olde Rikkert, Andy Haines, Ira Helfand, Richard Horton, Bob Mash, Arun Mitra, Carlos Monteiro, Elena N. Naumova, Eric J. Rubin, Tilman Ruff, Peush Sahni, James Tumwine, Paul Yonga, Chris Zielinski, Reducing the risks of nuclear war - The role of health professionals , Bleeding, Thrombosis and Vascular Biology: Vol. 2 No. 3 (2023)
- Nadim Tawil, Lata Adnani, Janusz Rak, Coagulome and tumor microenvironment: impact of oncogenes, cellular heterogeneity and extracellular vesicles , Bleeding, Thrombosis and Vascular Biology: Vol. 3 No. s1 (2024): 12th ICTHIC
- Maria J. Fernandez Turizo, Rushad Patell, Jeffrey I. Zwicker, Identifying novel biomarkers using proteomics to predict cancer-associated thrombosis , Bleeding, Thrombosis and Vascular Biology: Vol. 3 No. s1 (2024): 12th ICTHIC
- Luca Puccetti, Vincenzo Sammartano, Federico Caroni, Margherita Malchiodi, Paola Calzoni, Eleonora Franceschini, Lucrezia Galasso, Monica Bocchia, Safety of COVID-19 mRNA vaccination in patients with history of acquired hemophilia A: a case series , Bleeding, Thrombosis and Vascular Biology: Vol. 1 No. 3 (2022)
- Giancarlo Castaman, Gene transfer in hemophilia B: a big step forward , Bleeding, Thrombosis and Vascular Biology: Vol. 2 No. 2 (2023)
- Daniela Poli, Emilia Antonucci, Gualtiero Palareti, Roberto Facchinetti, Pietro Falco, Giuseppina Serricchio, Teresa Lerede, Lucilla Masciocco, Paolo Gresele, Sophie Testa, Major bleedings in mechanical prosthetic heart valves patients on Vitamin K antagonist treatment. Data from the PLECTRUM Study , Bleeding, Thrombosis and Vascular Biology: Vol. 1 No. 2 (2022)
- Matteo Guarascio, Gerardo Nicola Pititto, Alessia Abenante, Marco Paolo Donadini, Distal deep vein thrombosis: is there a way out of this dark forest? , Bleeding, Thrombosis and Vascular Biology: Vol. 3 No. 2 (2024)
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/btvb.2022.41
https://doi.org/10.4081/btvb.2022.41