Original Articles
Vol. 2 No. 3 (2023)
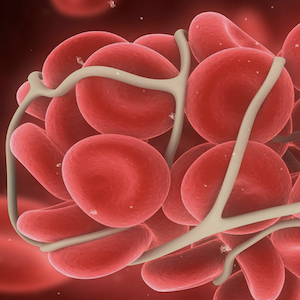
Descriptive analysis of patients positive for anti-phospholipid antibodies included in two Italian registries
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Received: 13 July 2023
Accepted: 20 September 2023
Accepted: 20 September 2023
843
Views
247
Downloads
Similar Articles
- Juan Eirís, Marina Suárez-Terrón, Pablo Granados, David Martínez-Campuzano, Ana Rosa Cid, Saturnino Haya, Santiago Bonanad, Allopurinol-induced acquired von Willebrand syndrome , Bleeding, Thrombosis and Vascular Biology: Vol. 2 No. 4 (2023)
- Silvia Cardi, Filippo Catalani, Luca Valerio, Stefano Barco, From rare to aware: confronting Lemierre syndrome , Bleeding, Thrombosis and Vascular Biology: Vol. 3 No. 3 (2024)
- Paolo Prandoni, New perspectives for prevention of the post-thrombotic syndrome , Bleeding, Thrombosis and Vascular Biology: Vol. 1 No. 1 (2022)
- CS07 | Endothelial dysfunction and impaired angiogenesis in Hermansky-Pudlak syndrome (HPS) type 1: studies with endothelial colony forming cells , Bleeding, Thrombosis and Vascular Biology: Special issues
- Luca Barcella, Chiara Ambaglio, Paolo Gritti, Francesca Schieppati, Varusca Brusegan, Eleonora Sanga, Marina Marchetti, Luca Lorini, Anna Falanga, Long-term persistence of high anti-PF4 antibodies titer in a challenging case of AZD1222 vaccine-induced thrombotic thrombocytopenia , Bleeding, Thrombosis and Vascular Biology: Vol. 2 No. 2 (2023)
- Ottavia Borghese, Claudio Vincenzoni, Commentary on “Preventive percutaneous coronary intervention versus optimal medical therapy alone for the treatment of vulnerable atherosclerotic coronary plaques (PREVENT): a multicenter, open-label, randomized controlled trial” , Bleeding, Thrombosis and Vascular Biology: Vol. 3 No. 2 (2024)
- Matteo Guarascio, Gerardo Nicola Pititto, Alessia Abenante, Marco Paolo Donadini, Distal deep vein thrombosis: is there a way out of this dark forest? , Bleeding, Thrombosis and Vascular Biology: Vol. 3 No. 2 (2024)
- Domenico Prisco, Irene Mattioli, Raffaele De Caterina, Alessandra Bettiol, The new era of anticoagulation: factor XI and XII inhibitors , Bleeding, Thrombosis and Vascular Biology: Vol. 2 No. 2 (2023)
- Giovanni Tiscia, Elvira Grandone, Talking about assisted reproductive techniques and thromboembolic risk: everything we always wanted to know , Bleeding, Thrombosis and Vascular Biology: Vol. 1 No. 2 (2022)
- Luca Puccetti, Vincenzo Sammartano, Federico Caroni, Margherita Malchiodi, Paola Calzoni, Eleonora Franceschini, Lucrezia Galasso, Monica Bocchia, Safety of COVID-19 mRNA vaccination in patients with history of acquired hemophilia A: a case series , Bleeding, Thrombosis and Vascular Biology: Vol. 1 No. 3 (2022)
1-10 of 14
Next
You may also start an advanced similarity search for this article.